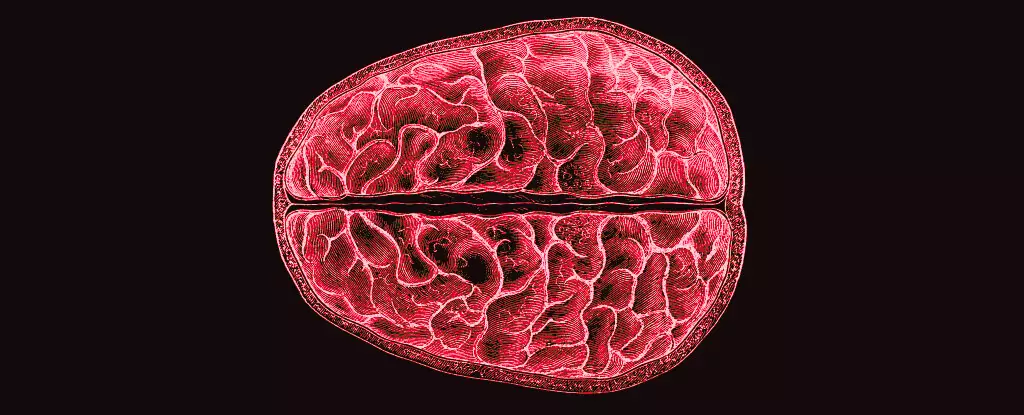
The menstrual cycle is often perceived merely as a physiological process associated with reproduction. However, emerging research sheds light on the intricate relationship between hormonal fluctuations during this cycle and their profound effects on the brain. A recent study conducted by a team of neuroscientists from the University of California Santa Barbara demands attention, as it uncovers how these hormonal changes can reshape brain structures, bringing new insights that could alter our understanding of women’s health.
Hormones are not just catalysts for reproductive events; they are active participants in the orchestration of neurological health and capacity throughout the menstrual cycle. Led by researchers Elizabeth Rizor and Viktoriya Babenko, the study tracked 30 menstruating women through various phases of their cycles. This rigorous examination was not merely a surface-level inquiry; it meticulously documented the brain’s structural changes as hormone levels ebbed and flowed. The findings, which indicated simultaneous modifications in both white matter microstructure and cortical thickness, challenge traditional views of hormonal effects localized to specific brain regions.
The research team posited that the implications of hormone-brain interactions extend much further than the well-known hypothalamic-pituitary-gonadal (HPG) axis. This insight opens up new avenues for exploring how these fluctuations might influence cognitive function and emotional regulation, particularly during the complex times of the menstrual cycle. As the prevalence of mental health issues related to hormonal shifts in women becomes more recognized, understanding these neurobiological dynamics is both timely and essential.
The Research Gap: Why So Little Focus on Menstrual Effects?
Despite the significant role that menstruation plays in millions of lives worldwide, scholarly exploration of its impact on brain function has been notably scarce. Predominantly, existing studies have dwelt on cognitive performance under hormonal influences rather than the biological underpinnings of those effects. The mystery of this research gap raises questions about societal attitudes towards women’s health and the historical underrepresentation of women’s experiences in clinical research.
The UCSB team’s findings foreshadow a potential shift in this narrative. They emphasize the need for expanded research on how hormonal fluctuations during menstruation affect brain structure and overall mental health. As the study suggests, the cyclical oscillation of the HPG-axis hormones doesn’t merely govern reproductive functions—they also wield substantial influence over the very architecture of the human brain.
Utilizing advanced MRI technology, Rizor and Babenko’s team undertook a thorough exploration of the brain at three different menstrual phases: menses, ovulation, and the mid-luteal phase. Their results indicate that as hormone levels rise and fall, both gray and white matter volumes adjust concurrently. Additional intriguing discoveries point out that these hormonal fluctuations not only alter the physical properties of the brain but also the dynamics of cerebrospinal fluid.
In instances where estrogen levels peak, particularly before ovulation, alterations in white matter suggest enhancements in information transport efficiency between brain regions. The study found that the production of follicle-stimulating hormone coincided with increased gray matter thickness, potentially indicating a relationship between hormonal cascades and cognitive processing capabilities. Conversely, the aftermath of ovulation sees the rise of progesterone, associated with increased brain tissue density but a decrease in cerebrospinal fluid volume, further complicating the narrative of hormonal impacts on mental stability.
The implications of this study are vast. Understanding the interplay between hormonal cycles and brain structure could lay the groundwork for future explorations into mental health issues that disproportionately impact women throughout their lives. Conditions ranging from premenstrual syndrome (PMS) to postpartum depression often remain inadequately addressed in terms of underlying biological mechanisms.
This study calls for renewed focus on women’s health research, urging a comprehensive approach that takes hormonal impacts into account. As science continues to unravel the complexities of the menstrual cycle, one can only hope that this newfound knowledge will catalyze discussions around better healthcare practices and broader societal understanding of women’s experiences. Ultimately, bridging the gap between hormonal changes and mental health stands as a critical frontier in neuroscience, with the potential to greatly enhance the quality of life for individuals who menstruate.

Leave a Reply