The medical world has long been striving to grow functional human organs outside the body, a quest that has proven to be elusive until recent advancements. A team of scientists from Harvard’s Wyss Institute for Biologically Inspired Engineering and John A. Paulson School of Engineering and Applied Science (SEAS) has made a significant breakthrough in this field. By 3D-printing vascular networks with interconnected blood vessels surrounded by smooth muscle cells and endothelial cells inside human cardiac tissue, they are paving the way for the manufacturing of implantable human organs.
Through the development of a new 3D bioprinting method known as ‘sacrificial writing in functional tissue’ (SWIFT) and coaxial SWIFT (co-SWIFT), the research team has managed to replicate the multilayer architecture of native blood vessels. The key innovation lies in a core-shell nozzle equipped with two independently controllable fluid channels for different ‘inks’ used in the printing process. By varying printing speed and ink flow rates, the size of the vessels can be adjusted, allowing for a more versatile and customizable approach.
To validate the effectiveness of the co-SWIFT method, the team successfully printed branching vascular networks in various cell-free matrices, including a transparent granular hydrogel matrix and uPOROS, a porous collagen-based material mimicking living muscle tissue. After printing the biomimetic vessels, a heating process enabled the removal of sacrificial gelatin core ink, resulting in open and perfusable vasculature.
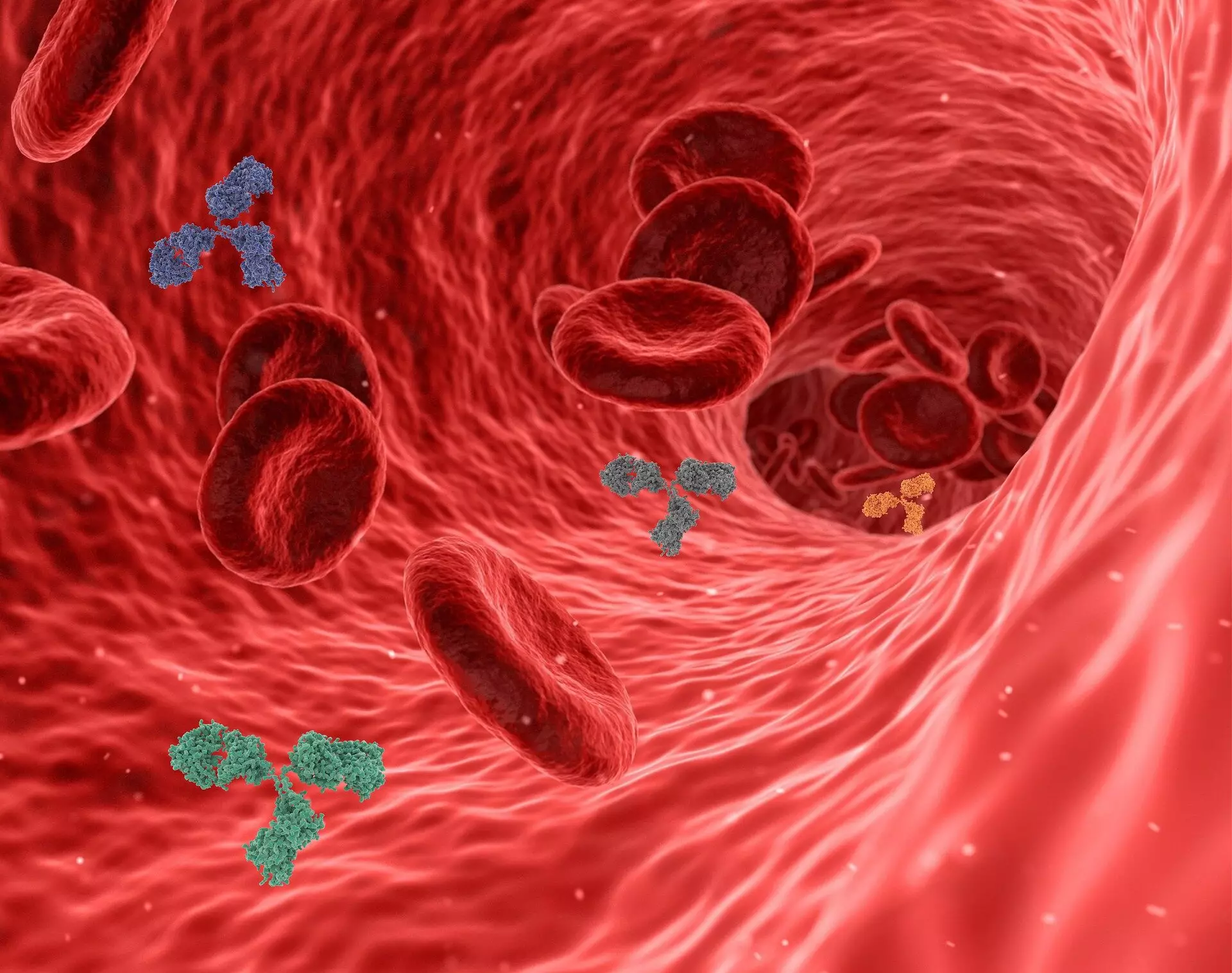
Moving to biologically relevant materials, the team infused the shell ink with smooth muscle cells and perfused endothelial cells into the vasculature. The engineered vessels displayed a remarkable decrease in permeability and exhibited live and functional vessel walls after perfusion. The team also integrated the printed biomimetic vessel network with cardiac organ building blocks (OBBs), creating functional heart tissue that responded to cardiac drugs and displayed synchronous beating.
The application of co-SWIFT extends to personalized medicine, as demonstrated by the team’s ability to 3D-print a model of a real patient’s left coronary artery vasculature into OBBs. This breakthrough opens up new possibilities for creating patient-specific, vascularized human organs. The potential for engineering self-assembled networks of capillaries and integrating them with 3D-printed blood vessel networks represents a promising direction for enhancing the structure and function of lab-grown tissues.
The research team, led by Wyss Founding Director Donald Ingber and Wyss Core Faculty member Jennifer Lewis, is committed to advancing the field of organ transplantation. Their vision includes the generation of self-assembled capillary networks to fully replicate human blood vessel structures, aiming to implant lab-grown tissues into patients successfully. While the road ahead is challenging, the team’s determination and creativity are driving innovation in the quest for functional living human tissues.
The development of 3D-printed vascular networks represents a groundbreaking achievement in the field of organ transplantation. By mimicking the architecture of native blood vessels and integrating living cells into engineered tissues, the potential for manufacturing implantable human organs is closer than ever before. As the research progresses, the future of personalized medicine and regenerative therapies looks brighter, offering hope for patients awaiting life-saving organ transplants.

Leave a Reply